Co-Occuring Disorders Guide for Dual Diagnosis

If you typed co-occuring into a search bar, you are not alone. Many people spell it this way when they are trying to understand something scary and confusing: what it means when mental health symptoms and addiction show up together.
The correct spelling is co-occurring, and in addiction and mental health care it usually refers to co-occurring disorders, sometimes called dual diagnosis or comorbidity.
This guide explains what people usually mean by “co-occuring,” the signs to look for, why it happens, and what effective, evidence-based treatment typically includes. If you are reading this for yourself or someone you love, you deserve support that treats the whole person, not just one diagnosis.
Important note: If you or someone else is in immediate danger, call 911. If you are in the U.S. and need urgent emotional support, call or text 988 for the Suicide and Crisis Lifeline.
What does co-occuring mean?
Co-occuring is a common misspelling of co-occurring. The word “co-occurring” simply means two or more conditions happen at the same time. (For a shorter definition-focused explanation, see this breakdown of what “co-occuring” means in dual diagnosis care.)
In behavioral health, “co-occurring” most often means:
- A substance use disorder (SUD) such as alcohol, opioids, methamphetamine, cocaine, cannabis, or benzodiazepines, and
- A mental health disorder such as depression, anxiety, PTSD, bipolar disorder, ADHD, schizophrenia, or other conditions.
You might also hear the term comorbidity. That is a broad medical term meaning a person has more than one diagnosis at the same time. In real life, what matters is that both conditions affect each other, and treatment works best when care is coordinated.
Co-occurring vs dual diagnosis vs comorbidity
These terms overlap, and different clinicians use them differently. Here is a practical way to think about them:
- Dual diagnosis often means one mental health disorder plus one substance use disorder.
- Co-occurring disorders is commonly used the same way, but it can also include multiple mental health diagnoses and other health conditions along with substance use.
- Comorbidity is the broader medical term for having more than one disorder at the same time.
No matter which phrase you see, the key is the same: treating only one condition often leaves relapse triggers and symptoms untreated. You can also read this overview of co-occuring disorders and dual diagnosis care for a treatment-centered view.
How common are co-occurring disorders?
Co-occurring mental health and substance use challenges are common in the U.S., which is one reason many treatment programs now screen for both.
SAMHSA’s National Survey on Drug Use and Health tracks substance use, mental health, and treatment access each year. Their 2023 NSDUH release highlights that the survey includes estimates for mental illness co-occurring with substance use and substance use disorders, and also reports on treatment needs across the country.
In plain terms: if you are dealing with both anxiety or depression and alcohol or drug use, it is not rare, and it is not a personal failure. It is a health issue that can be treated.
Why co-occurring disorders happen
There is not one single cause. Co-occurring disorders usually develop from a mix of biology, life experience, environment, and how the brain responds to stress and substances.
1) Self-medication
Many people use alcohol or drugs to numb panic, trauma memories, grief, low mood, insomnia, or racing thoughts. Substances can feel like they “work” in the short term, but over time they tend to worsen sleep, anxiety, depression, irritability, and overall stability.
2) Substances can trigger or worsen mental health symptoms
Alcohol and drugs can change brain chemistry and stress hormones. Stimulants can increase anxiety and paranoia. Heavy alcohol use can contribute to depression and disrupted sleep. (Related reading: how alcohol affects behavior and thinking.) Cannabis can worsen anxiety in some people and can increase risk of psychosis symptoms in vulnerable individuals.
3) Shared risk factors
Genetics, family history, trauma, chronic stress, unstable housing, discrimination, and untreated medical problems can raise risk for both mental health disorders and substance use disorders.
4) Gaps in diagnosis and care
Sometimes one condition gets treated while the other goes unnoticed. For example, a person might receive antidepressants but not get support for heavy drinking, or they might complete detox but never get evaluated for PTSD. When care is fragmented, symptoms can persist and relapse becomes more likely.
Common examples of co-occurring disorders
Every person’s story is unique, but some combinations show up often in treatment settings:
- Alcohol use disorder with depression or anxiety
- Opioid use disorder with PTSD or depression
- Methamphetamine or cocaine use with anxiety, depression, or psychosis symptoms
- Benzodiazepine misuse with panic disorder or insomnia
- Trauma history with multiple substances
- Bipolar disorder with alcohol or stimulant use
Signs you might be dealing with co-occuring disorders
Co-occurring disorders can be hard to recognize because symptoms overlap. Some people do not know what came first. Others feel shame about substance use and only talk about anxiety or depression, or the reverse.
Substance use disorder signs
- Using more than intended or longer than planned
- Trying to cut down and not being able to
- Withdrawal symptoms when you stop or reduce use
- Cravings or constant preoccupation with getting or using
- Continuing use despite relationship, work, or health consequences
- Mixing substances, driving impaired, or other risky use
Mental health warning signs
- Persistent sadness, numbness, hopelessness, or losing interest in life
- Ongoing anxiety, panic attacks, or constant worry
- Trauma symptoms like nightmares, flashbacks, and hypervigilance
- Intense mood swings, irritability, or periods of unusually high energy
- Difficulty concentrating, changes in sleep or appetite
- Thoughts of self-harm or suicide
A common clue: the cycle
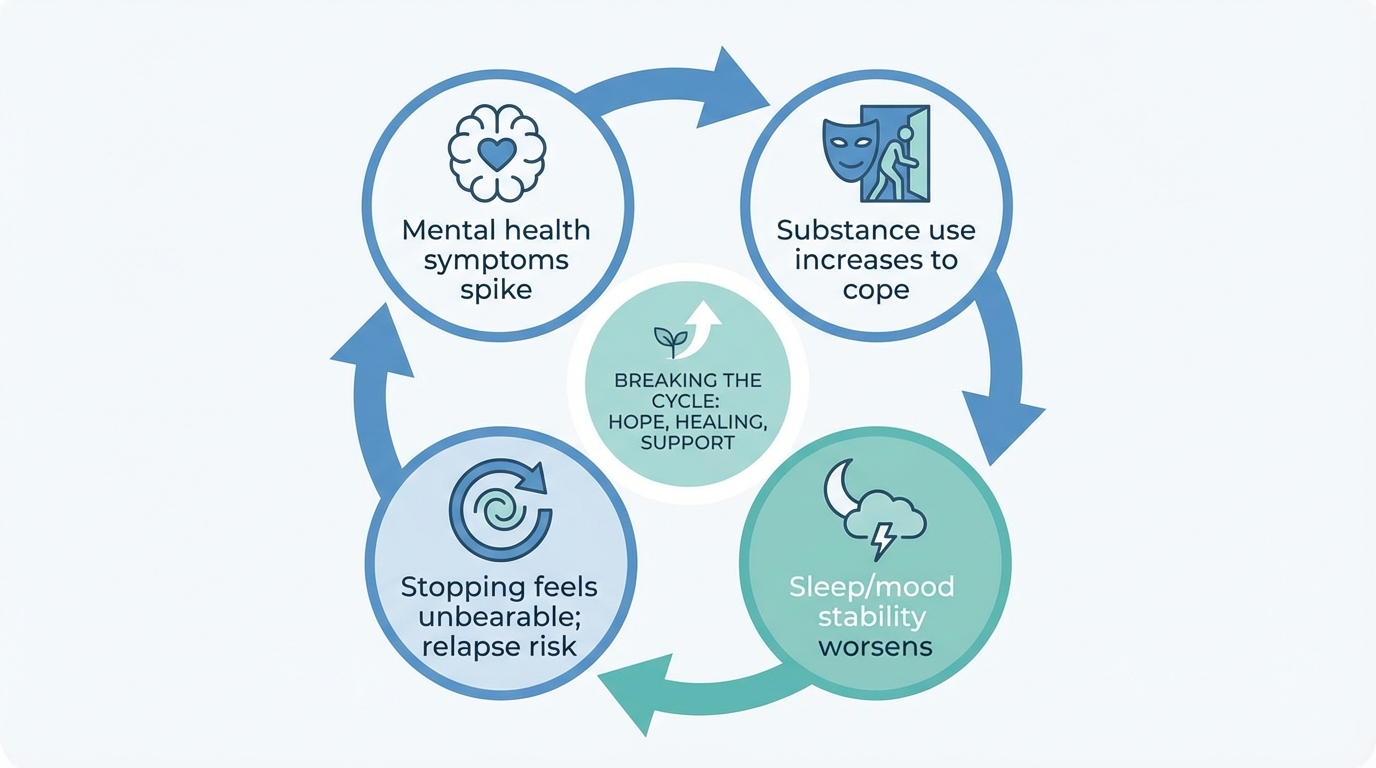
Many people describe a pattern like this:
- Mental health symptoms spike
- Substance use increases to cope
- Substance use worsens sleep, mood, and stability
- Trying to stop feels unbearable, then relapse happens
If you recognize this cycle, it does not mean you are weak. It often means you need integrated treatment that supports both conditions at the same time.
Why treating only one condition often does not work
It is possible to make progress focusing on one issue first, especially if there is immediate risk like overdose or severe withdrawal. But long-term recovery is harder when the other condition is ignored.
- If a person completes treatment for substance use but PTSD goes untreated, trauma triggers can drive relapse.
- If someone takes medication for anxiety or depression but continues heavy drinking, the alcohol can blunt medication effects and worsen sleep and mood.
- If someone has bipolar disorder and is using stimulants, mood stabilization becomes much more difficult.
That is why many experts recommend coordinated, integrated care for dual diagnosis.
What effective co-occurring disorders treatment looks like

There is no one-size-fits-all plan. But strong dual diagnosis treatment usually includes the elements below.
1) Full assessment and screening
A quality program or clinician should take time to assess:
- Which substances are being used, how often, and in what situations
- Withdrawal risk and medical history
- Mental health symptoms, including trauma history
- Medication history and possible interactions
- Safety concerns, including self-harm or suicide risk
Because substances can mimic mental health symptoms (and vice versa), diagnoses sometimes become clearer after a period of stabilization. Good clinicians re-evaluate over time instead of rushing to label you.
2) Medically supported detox when needed
Detox can be a safer starting point for certain substances, especially:
- Alcohol (withdrawal can be dangerous without medical support)
- Benzodiazepines (withdrawal can cause seizures and severe anxiety)
- Opioids (withdrawal is rarely life-threatening but can be intense and destabilizing)
Detox alone is not treatment, but it can create enough stability to begin therapy, medication management, and long-term planning. If you’re comparing programs, this can also help: what rehab facilities typically provide (and how they support recovery).
3) Integrated therapy for addiction and mental health
Evidence-based approaches often include:
- Cognitive Behavioral Therapy (CBT) to build coping skills for triggers, cravings, and unhelpful thought patterns.
- Dialectical Behavior Therapy (DBT) skills for emotional regulation, distress tolerance, and impulsivity.
- Motivational interviewing to strengthen readiness for change without shame or pressure.
- Trauma-informed care to avoid re-traumatization and build safety and stabilization first.
Trauma therapy may happen in phases. Many programs start with stabilization and coping skills before deeper trauma processing, especially if substance use has been heavy or recent.
4) Medication management, when appropriate
Medications can be a helpful tool for many people with co-occurring disorders. Depending on the situation, a clinician may consider:
- Medications for depression, anxiety, bipolar disorder, ADHD, or psychotic symptoms
- Medications for alcohol use disorder (to reduce cravings or support abstinence)
- Medications for opioid use disorder (such as buprenorphine or methadone) that reduce overdose risk and support recovery
Medication should be monitored closely, especially if there is a history of misuse or if multiple sedating medications could increase overdose risk.
5) The right level of care
Dual diagnosis treatment can happen at different levels depending on need, safety, and support at home:
- Inpatient or residential treatment for higher symptom severity, unstable housing, or high relapse risk
- Partial hospitalization programs (PHP) for structured daytime care with evenings at home or in supportive housing
- Intensive outpatient programs (IOP) for ongoing therapy several days per week
- Outpatient therapy and psychiatry for stable situations with strong support
Many people step down through levels of care, rather than doing one program and being “done.” Recovery often works best when support matches how life changes over time. If you’re trying to understand what inpatient care means in practice, ALT has a helpful explainer: inpatient vs. outpatient treatment (what’s the difference?).
6) Relapse prevention and long-term support
Co-occurring disorders are rarely solved by willpower alone. Long-term recovery planning often includes:
- A relapse prevention plan (warning signs, triggers, coping strategies, and a “what to do if I slip” plan)
- Peer support (mutual aid groups, recovery communities, or other nonjudgmental support spaces)
- Ongoing therapy and psychiatric follow-up
- Support for sleep, nutrition, movement, and stress management
- Help with housing, job support, and legal or family stressors when needed
If you need structured “in-between” support after residential care, a transitional setting can help some people stay stable while building routines. ADR explains options here: what a halfway house is and how it supports recovery.
When co-occurring symptoms are an emergency
Get immediate help if you notice any of the following:
- Overdose risk, especially mixing opioids with alcohol or benzodiazepines
- Severe withdrawal symptoms such as confusion, seizures, or hallucinations
- Psychosis symptoms (paranoia, hearing voices) or extreme agitation
- Inability to care for yourself safely
- Thoughts of suicide or self-harm
If you are in the U.S., you can call or text 988 for the Suicide and Crisis Lifeline. If you believe someone’s life is in immediate danger, call 911.
Practical next steps if you suspect co-occuring disorders
If you are unsure where to start, these steps can help you move forward without having to figure everything out at once:
- Write down what you are noticing – mood changes, panic, trauma triggers, sleep issues, cravings, withdrawal symptoms, and what substances are involved.
- Ask specifically for a dual diagnosis assessment when contacting a provider or treatment program.
- Prioritize safety – especially if withdrawal risk, overdose risk, or suicidal thoughts are present.
- Look for integrated treatment – care teams that address mental health and addiction together rather than separately.
- Involve one supportive person if possible – a friend, partner, family member, or advocate who can help you make calls and attend appointments.
How to choose a co-occurring disorders program
When you call a treatment program or clinician, it can help to ask clear questions. Here are a few that often reveal whether a program truly supports dual diagnosis:
- Do you provide integrated treatment for mental health and substance use disorders?
- Is there psychiatric care available for evaluation and medication management?
- How do you handle trauma and PTSD? Is your approach trauma-informed?
- What happens after discharge – do you help with aftercare planning?
- Do you coordinate care with my current therapist, doctor, or family (with permission)?
Trust your instincts. If a provider dismisses your mental health concerns or treats addiction as purely a discipline problem, it is okay to keep looking.
Frequently Asked Questions
What is co-occuring?
“Co-occuring” is a common misspelling of “co-occurring.” In addiction and mental health, co-occurring usually means a person has both a substance use disorder and a mental health disorder at the same time.
Is co-occurring the same as dual diagnosis?
Often, yes. Dual diagnosis typically means one mental health disorder plus one substance use disorder. Co-occurring disorders is a broader term that can include multiple mental health diagnoses alongside substance use.
What are signs of co-occurring disorders?
Common signs include difficulty cutting down on alcohol or drugs, withdrawal symptoms, cravings, and persistent mental health symptoms like depression, anxiety, trauma symptoms, mood swings, or suicidal thoughts. Many people notice a cycle where mental health symptoms trigger substance use and substance use worsens mental health.
What kind of treatment works best for co-occurring disorders?
Integrated treatment is considered best practice. That usually includes a comprehensive assessment, therapy that addresses both conditions (such as CBT or DBT), trauma-informed care when relevant, and medication management when appropriate. The right level of care can range from outpatient to residential treatment.
Can I recover if I have both addiction and a mental health disorder?
Yes. Recovery is possible, even when symptoms feel tangled together. Many people do best with coordinated care, consistent follow-up, and a long-term support plan that includes therapy, community support, and relapse prevention strategies.
Need Help Now?
If you or someone you love is struggling with addiction, help is available 24/7.
- SAMHSA National Helpline: 1-800-662-4357 (free, confidential, 24/7)
- Crisis Text Line: Text HOME to 741741
- National Suicide Prevention Lifeline: 988
Recovery is possible. Take the first step today.
Find Help Near You
National Consumer Support & Litigation
110 N Lincoln Ave, Corona, CA 92882
Phone: (951) 582-2018